Urinary Bladder Cancer
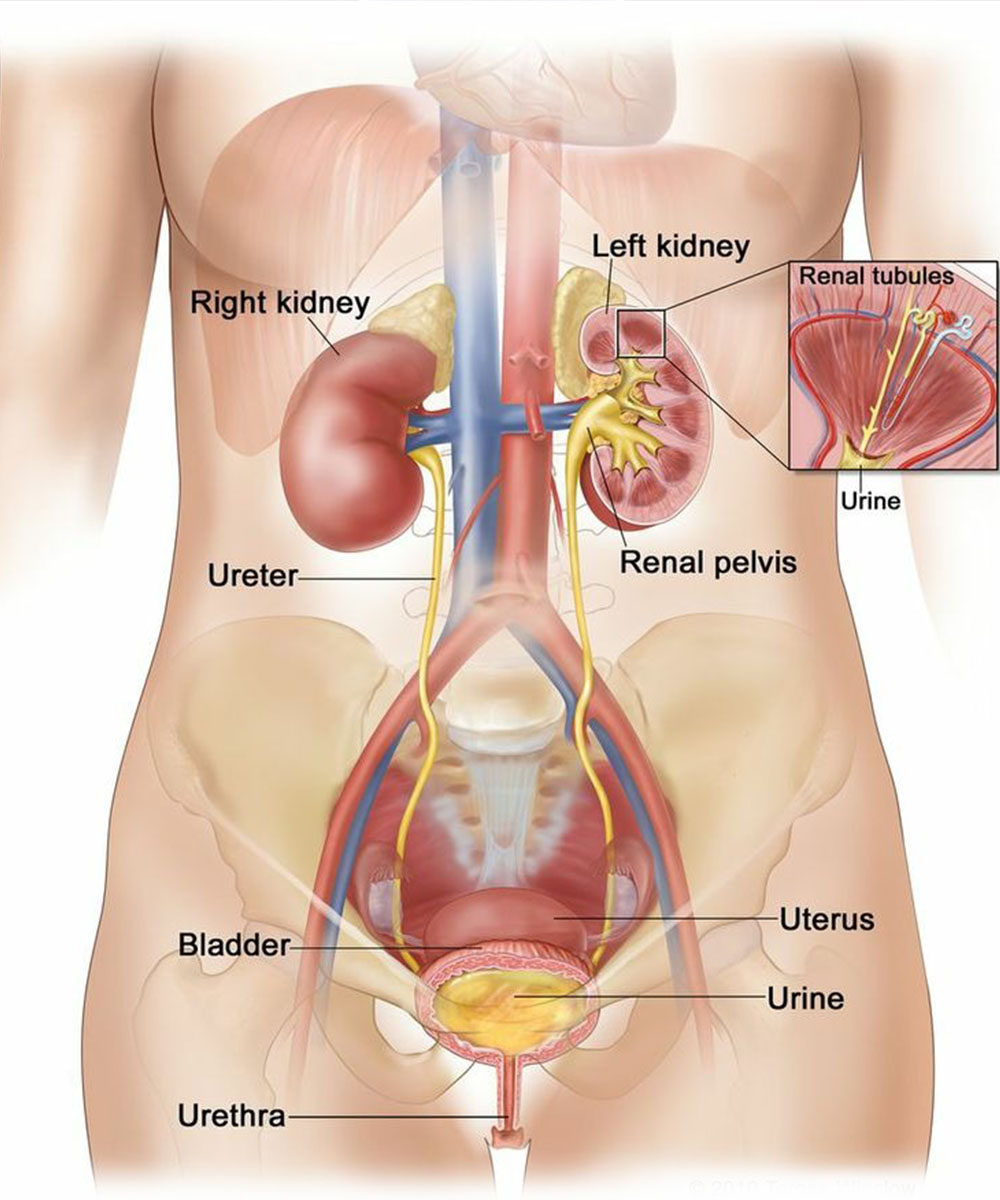
Cancer of the urinary bladder is the abnormal condition of the urothelial cells that form the inner lining of the urinary bladder, which then spreads into the deeper tissues of the urinary bladder wall after a period of time.
Bladder cancers usually have a tendency to remain confined to the inner layers (also called the mucosal layer) for the longest period of time.
As cancer advances to further stages, it spread to the neighbouring lymph nodes and subsequently to other body parts
Symptoms of Urinary Bladder Cancer:
The symptoms of urinary bladder cancer include the following:
Types of Urinary Bladder Cancer

Diagnostics Facilities
Advanced Cancer Diagnostics
Advanced Cancer Treatment
General Diagnostic Facilities
Causes of Urinary Bladder Cancer
Factors that increase the risk of contracting urinary bladder cancer include:
- Smoking: Smoking cigarettes, cigars, or pipes. Tobacco smokers have a three-fold increased risk of contracting bladder cancer as compared to non-smokers and even ex-smokers have a two-fold increased risk.
- Exposure to chemicals: Exposure to chemicals like aromatic amines, aniline dyes, nitrites and nitrates. Usually, workers in industries manufacturing dyes, rubber, leather, textiles and paint products have an increased risk of getting exposed to these chemicals.
- Chronic irritants: These include individuals with recurrent urinary tract infections, long-term catheterization, and parasitic infection with Schistosoma haematobium (Bilharziasis).
- Long-term treatment with drugs like cyclophosphamide: Long-term cyclophosphamide administration for treatment of other cancers or rheumatological conditions, particularly in patients with bladder outlet obstruction.
- Pelvic radiation: Radiation to the pelvic region also increases one’s risk of contracting bladder cancer.
- Personal or family history of cancer: If an immediate family member (siblings/parents) has been affected with bladder cancer, it increases the individual’s risk of having the same genetic mutations and thus contracting bladder cancer. A family history of Lynch syndrome [hereditary nonpolyposis colorectal cancer (HNPCC)], increases the risk of cancer in the urinary system.
When to see the Doctor?
The symptoms can appear in different forms as mentioned above and hence, if you are experiencing any of these symptoms, especially for more than 2-3 weeks, it would be best to consult a doctor.

Prevention of Urinary Bladder Cancer

Tests for urinary bladder cancer
On consultation with a specialist, the following tests may be carried out:
- A physical exam: A thorough physical examination will be carried out, after taking into account a detailed history of your symptoms.
- Ultrasound: An abdominal ultrasound is initially done to look for the presence of suspicious thickening or masses in the urinary bladder.
- CT scan: A CT scan of the chest, abdomen and pelvis is done to determine the stage of disease; which in turn will help decide the best treatment sequence for the patient.
- MRI scan: An MRI scan may sometimes be conducted to confirm or rule out suspicious findings on a CECT scan.
- PET CECT scan: A PET CT scan is suggested in advanced or recurrent cases to rule out the spread of cancer to other sites, eg. lungs, liver, bone, etc.
- Cystoscopy: A cystoscope (a thin tube with a camera at the tip) is inserted into the tract to assess the size, number and location of the urinary bladder tumours. This procedure is usually carried out as a daycare procedure under general anaesthesia.
- Biopsy or TURBT: Biopsy or complete tumour resection – Trans Urethral Resection of Bladder Tumor (TURBT) is conducted at the time of cystoscopy in cases of superficial tumours. The detailed biopsy/TURBT report helps determine the treatment approach for the patient.
- Urine cytology: Urine samples are tested in all patients with suspected urinary bladder cancer to rule out the presence of free-floating cancerous cells in urine.

Treatment for urinary bladder cancer
The treatment for bladder cancer depends upon the stage and type of cancer.
Bladder cancer surgery: A few approaches to bladder cancer surgery include:
Transurethral resection of bladder tumour or TURBT: It is a procedure to diagnose as well as remove bladder cancers, which are restricted to the inner layers of the bladder. This procedure involves passing an electric wire loop through a cystoscope into the bladder to remove the tumour completely. This procedure is done through the urethra to not cause any damage to the abdomen.
Cystectomy:
This means the removal of the bladder surgically, which may be partial or radical:
- Partial cystectomy: In this process, only a part of the bladder affected by tumours along with a margin of normal bladder is removed. This is done in very selected patients with small tumours in the upper part (dome) of the bladder.
- Radical cystectomy: In this process, the entire bladder is removed along with the surrounding lymph nodes. In men, it involves the removal of the prostate and seminal vesicles. In women, it involves the removal of the uterus, ovaries and part of the vagina.Radical cystectomy is performed via open surgery or through laparoscopic or robotic procedures. After radical cystectomy, reconstruction is performed using the following methods:
- Neobladder reconstruction: Removal of the bladder in the radical cystectomy process eliminates the reservoir for the urine in the body hence, a neobladder(new bladder) is constructed in the form of a sphere using a part of the intestine. The ureters from both kidneys are anastomosed to the upper part of the neobladder, with the urethra anastomosed to the lower part, facilitating the normal urination process in most people. In some cases, people face difficulty emptying the bladder and require a catheter periodically to drain all the urine from the neobladder, called self-catheterization, which is taught to the patients by the treating doctors.
- Ileal conduit: This is a type of urinary diversion wherein a tube called ileal conduit is constructed from the intestine. The ureters from both kidneys are anastomosed to the ileal conduit on one side and the other end is connected to the urostomy bag through an opening in the abdominal wall, redirecting urine after bladder removal. Patients are trained to empty and change the urostomy bags periodically.
Chemotherapy:
Chemotherapy in the form of injections is suggested depending on the stage of the disease.
- Adjuvant chemotherapy: In this process, chemotherapy is given after surgery, consisting of 6 cycles, wherein 1 cycle represents a duration of 2-3 weeks.
- Neoadjuvant chemotherapy: In this process, chemotherapy is given before surgery, wherein 3 cycles are given before surgery, where each cycle represents a duration of 3 weeks and the remaining 3 cycles are then given as adjuvant chemotherapy after surgery.
- Intravesical chemotherapy: In this process, chemotherapy drugs, usually Mitomycin C, are injected into the bladder using a thin tube which is passed from the urethra into the bladder immediately after TURBT and retained for a certain period of time before being drained. This procedure is proven to minimize the recurrence of bladder cancer.
Intravesical therapy:
Intravesical BCG is often recommended after resection of the bladder, with early-stage bladder cancer employing the TURBT procedure (mentioned earlier). This procedure uses the bacillus Calmette-Guerin (BCG), a vaccine developed against tuberculosis that activates the immune system against bladder cancer cells, and the treating doctor decides the schedule for administering intravesical BCG.
Radiation therapy:
Radiation therapy, in the form of Adjuvant radiation, is given after surgery, especially in patients with positive margins. Radiation therapy may also be given along with chemotherapy (Definitive chemo-radiation) as a definitive treatment in some patients to preserve their bladder or before surgery (Neoadjuvant chemo-radiation) in advanced cases of bladder cancer to minimize tumour size.
Targeted therapy:
Targeted therapy uses drugs to target specific proteins within the cancer cells to eliminate them. For example, Erdafitinib targeting FGFR2/3 protein in bladder cancer cells is suggested for treating advanced bladder cancers.
Immunotherapy:
In advanced cases, biological therapy or immunotherapy is suggested as a treatment approach. Immunotherapy targets the cells that affect the body’s immune response and helps the body destroy cancer cells.
Doctors

Dr. Shreedhar G K

Dr. Saravana Rajamanickam

Dr. Karthick Rajamanickam

Dr. N. Kathiresan