Pancreatic Cancer
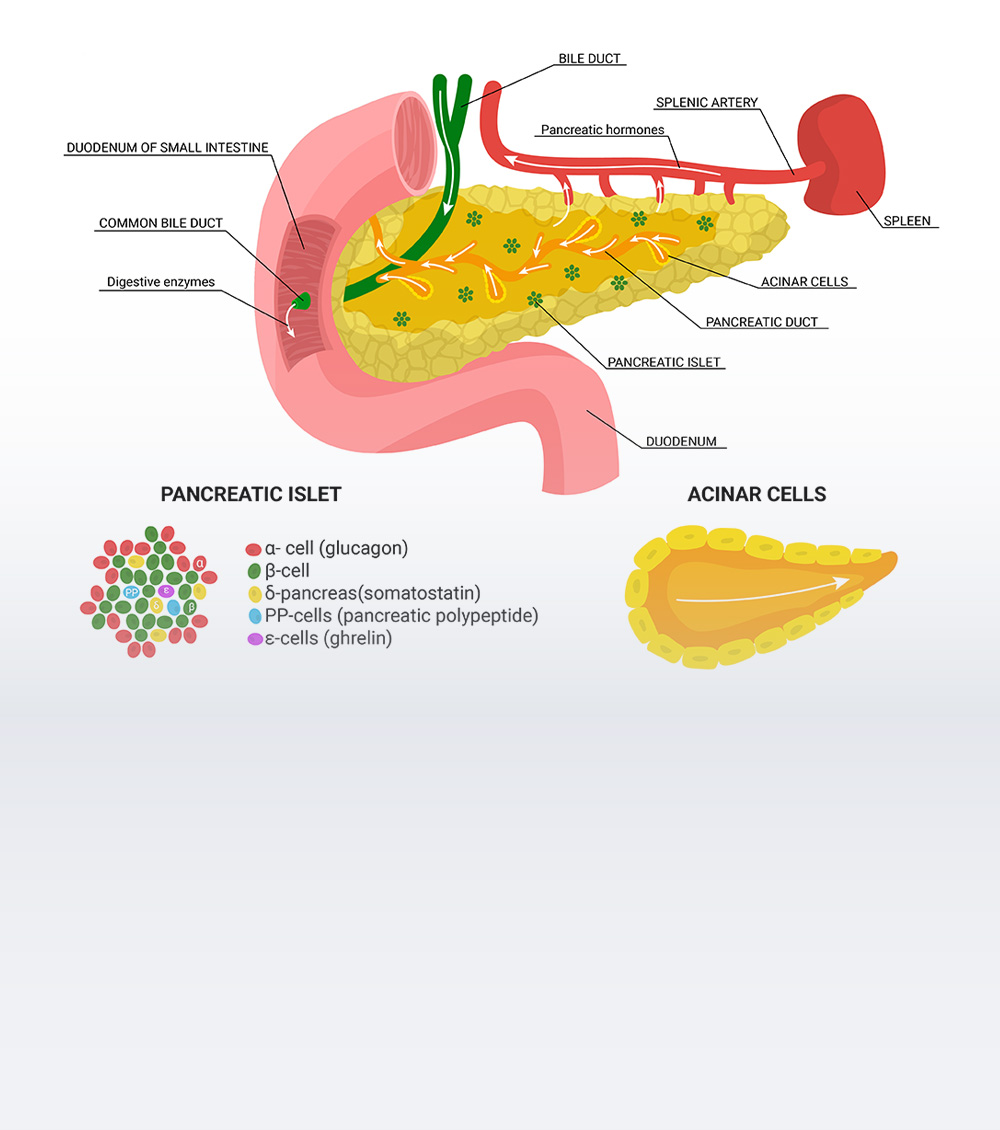
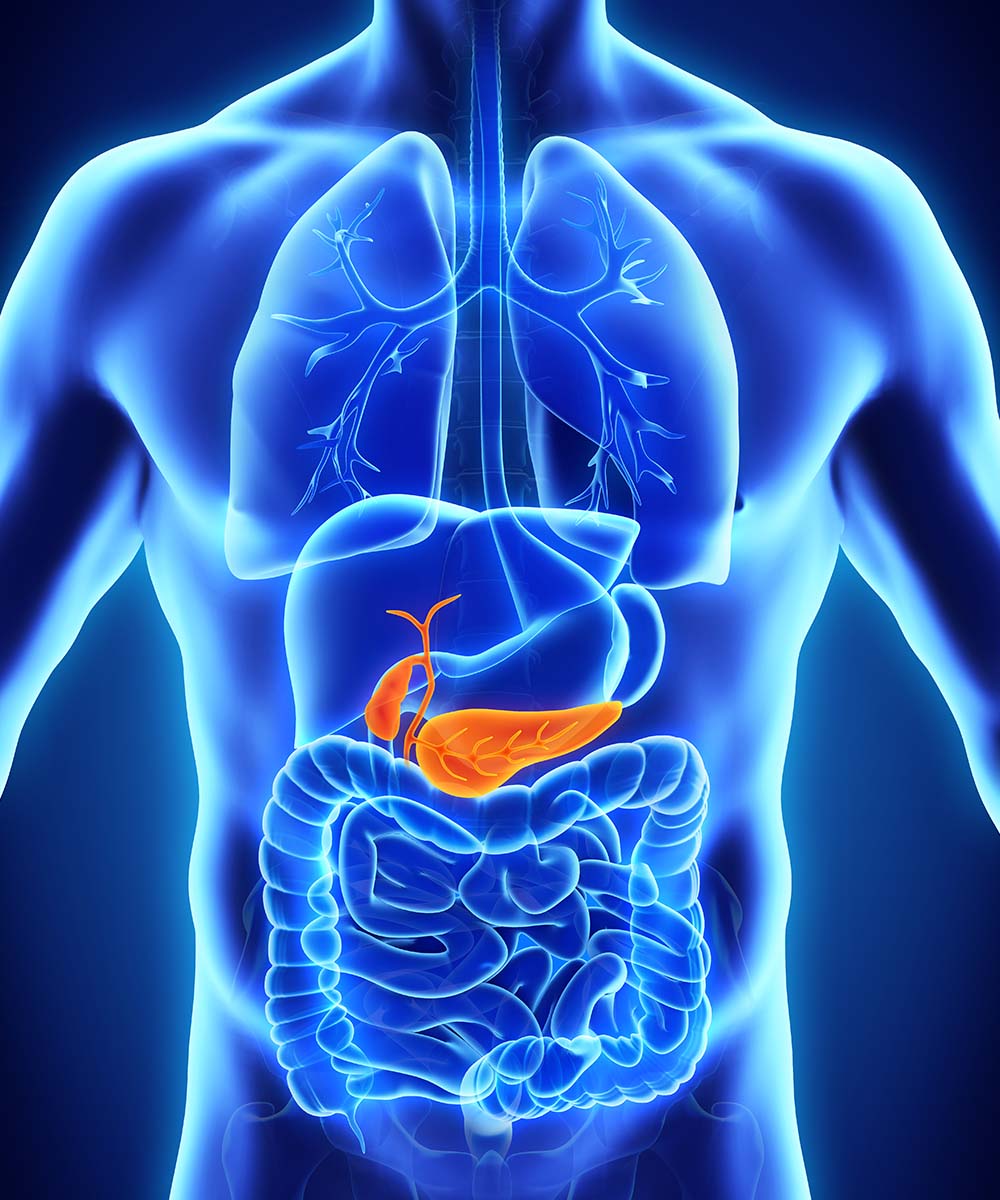
The pancreas is an elongated organ located posteriorly, below the stomach within the curve of the upper part of the small intestine, called the duodenum and comprises two types of glands the exocrine and endocrine glands.
The exocrine gland plays an important role in the digestion of fats, proteins and carbohydrates, by secreting digestive pancreatic juices and the endocrine gland helps in keeping the blood sugar levels under control by secreting insulin. Pancreatic cancer originates in the tissues of the pancreas located behind the lower portion of the stomach and is relatively more common in men than in women.
Symptoms of Pancreatic Cancer:
The symptoms of pancreatic cancer may include:
Types of Pancreatic Cancer
Exocrine pancreatic cancer:
This form of cancer is more common and includes:
- Pancreatic ductal adenocarcinoma: accounts for 90% of the cases of pancreatic cancer, it arises from the cells lining the ducts of the pancreatic glands and is of the following types.
- Squamous cell carcinoma
- Adenosquamous cell carcinoma
- Colloid carcinoma
Endocrine pancreatic cancer:
These are also called neuroendocrine or islet-cell tumours. These tumours can be ‘functional’ i.e. they secret extra amounts of hormones such as insulin, glucagon, and gastrin, that cause different signs and symptoms or ‘non-functional’ i.e. they do not secrete extra hormones. These include:
- Endocrine pancreatic cancer: These are also called neuroendocrine or islet-cell tumours. These tumours can be ‘functional’ i.e. they secret extra amounts of hormones such as insulin, glucagon, and gastrin, that cause different signs and symptoms or ‘non-functional’ i.e. they do not secrete extra hormones. These include:
- Gastrinomas (excess secretion of gastrin hormone)
- Glucagonomas (excess secretion of glucagon hormone)
- Insulinomas (excess secretion of insulin hormone)
- Somatostatinomas (excess secretion of somatostatin hormone)
- ‘VIP’ omas (excess secretion of Vasoactive intestinal peptide)

Diagnostics Facilities
Advanced Cancer Diagnostics
Advanced Cancer Treatment
General Diagnostic Facilities
Causes of Pancreatic Cancer
Factors that increase the risk of pancreatic cancer include:
- Smoking
- Diabetes
- Chronic inflammation of the pancreas (pancreatitis)
Family history of pancreatic cancer or genetic syndromes in families like BRCA2 gene mutation, Lynch syndrome and Familial atypical mole-malignant melanoma (FAMMM) syndrome is associated with an increased risk of pancreatic cancer.
- Obesity
- Older age
When to see the Doctor?
The symptoms and characteristics can vary in individuals; hence it is best advised to consult our specialists to rule out cancer possibilities as a preventive measure if you are experiencing a combination of any of these symptoms.
Prevention of Pancreatic Cancer
Tests for Pancreatic Cancer
Treatment for Pancreatic Cancer
Surgery
Surgical procedures to remove cancer include:
Chemotherapy
Chemotherapy in the form of injections or tablets may be suggested depending on the stage of the disease.
Chemo-radiation
Chemotherapy can also be recommended along with radiation treatment; called concurrent chemo-radiotherapy, and can be given in a neoadjuvant or adjuvant treatment approach.
Radiation therapy
Radiation therapy is given alone or in combination with chemotherapy depending upon the surgical histopathological report. In some cases, concurrent chemo-radiation is the only treatment approach, in patients with locally advanced disease wherein surgical resection cannot be performed safely.
Targeted therapy
Targeted therapy uses drugs to target specific proteins within the cancer cells, to kill them. For example, Trastuzumab targeting Her2neu protein in pancreatic cancer cells expressing Her2neu protein may be suggested.
Immunotherapy
In advanced cases, biological therapy or immunotherapy may be suggested for treatment. Immunotherapy targets the cells, which affect the body’s immune response and helps the body in killing cancer cells.
Doctors

Dr. Saravana Rajamanickam

Dr. Deepti Mishra

Dr. Aruna Prabhu

Dr. Bhavesh Poladia